Have you ever typed “isofegas pain” or “isofegas meaning” into a search bar, feeling a bit of that burning sensation in your chest or throat? If so, you’re definitely not alone. I did the exact same thing years ago, frustrated by constant heartburn I blamed on spicy food. That search, often a misspelling of the word esophagus (which comes from the Greek “oisophagos,” meaning “gullet”), is usually a first cry for help from a part of our body we rarely think about until it starts complaining.
Let’s talk about that complaint department – your esophagus. This guide won’t just define a term; it will walk with you through understanding this vital “food pipe,” why it might be causing you grief, and what you can actually do about it. Consider this a chat with a friend who’s been there, learned a lot from doctors and personal trial-and-error, and wants to share it in plain English.
What Exactly is the Esophagus? Let’s Get Acquainted.
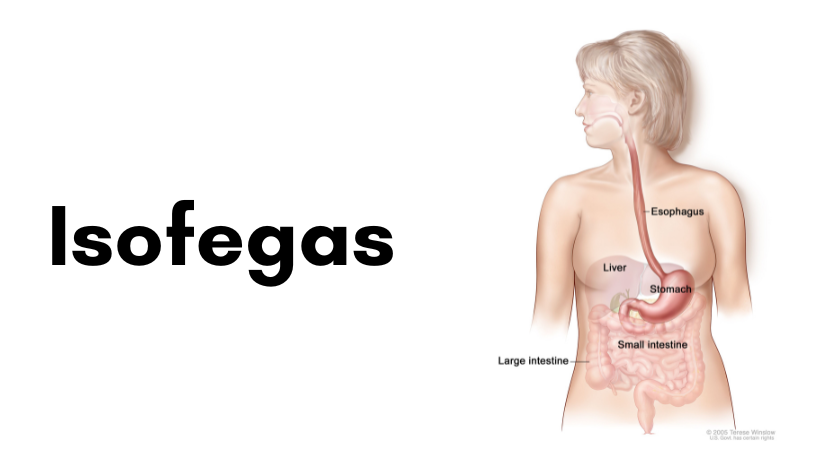
First things first, let’s clear the air. “Isofegas” is almost certainly a search for the esophagus. Think of it as the body’s dedicated food highway. It’s the muscular tube, about 10 inches long in most adults, that connects the back of your throat to your stomach. Its entire job is to be a reliable conveyor belt.
But here’s the fascinating part I never appreciated: it’s an active conveyor belt. When you swallow, it’s not just gravity doing the work. The esophagus uses a elegant, wavelike motion called peristalsis. It’s like squeezing a tube of toothpaste from the bottom up, but the squeeze is a gentle, coordinated muscle contraction that pushes food and liquid downward no matter if you’re standing, sitting, or even upside down (though I don’t recommend eating that way!).
At the very bottom of this tube, where it meets your stomach, sits a critical piece of anatomical engineering: the Lower Esophageal Sphincter (LES). Imagine this as a smart, one-way valve or a tight ring of muscle. Its job is to open just enough to let food pass into the stomach and then snap tightly shut to prevent the stomach’s very acidic contents from splashing back up. The entire harmony of your digestive system relies on this valve closing properly.
When the Harmony Breaks Down: Understanding the “Pain” in Your Search
When people search for “isofegas” issues, they are almost always feeling the consequences of a system under strain. The most common culprit is a malfunction of that clever LES valve.
If the LES is weak, relaxes at the wrong times, or is pressured from below, it doesn’t seal perfectly. This allows stomach acid, which is powerful enough to break down food, to creep back up into the delicate lining of the esophagus. This is acid reflux. Think of it as chemical splashback. That burning sensation in your chest (heartburn) or the sour taste in your throat is literally stomach acid where it doesn’t belong.
Now, if this happens occasionally, it’s normal. A rich meal, eating too late, or intense stress can cause a one-off episode. But when it becomes a frequent, twice-a-week nuisance, it graduates to a condition called GERD – Gastroesophageal Reflux Disease. This is where the real concern begins, because chronic acid exposure is like constantly bathing the esophagus in a harsh substance it wasn’t designed to handle.
The inflammation from this can lead to esophagitis (a swollen, sore esophagus, making swallowing painful). Over years, in some people, the body tries to protect itself by changing the lining of the esophagus to be more like stomach lining—a condition called Barrett’s Esophagus, which requires careful monitoring.
Other common issues behind “esophageal pain” include muscle spasms (which feel like a sudden, painful squeezing in your chest), hiatal hernia (where part of the stomach pushes up through the diaphragm, hindering the LES’s work), and, of course, infections or sensitivities.
Taking Back Control: Daily Habits for a Soothed Esophagus
The best news in all of this? Many aspects of esophageal health are within your control. Medicine has its place, and we’ll get to that, but lifestyle is the cornerstone. I learned this the hard way after relying on antacids for months.
1. Rethink Your Plate (and Your Portions): It’s not just about “spicy food.” Common triggers are acidic foods (tomatoes, citrus), caffeine, chocolate, mint, fatty foods, and alcohol. But here’s my personal opinion: the quantity and timing of eating often matter more than any single food. A huge meal fills your stomach, creating immense pressure that can blow open the LES valve. My game-changer was switching to smaller, more frequent meals. Eating until I was just satisfied, not stuffed, made a dramatic difference.
2. Become Best Friends with Gravity: Give your body time to process food before lying down. I made a firm rule: no eating within 3 hours of bedtime. If you need a snack, make it something light like a few crackers. If nighttime reflux is a problem, try elevating the head of your bed by 4-6 inches. Use sturdy blocks under the bed frame or a specialized wedge pillow. Piling up regular pillows often just bends you at the waist and can make pressure worse.
3. The Weight Connection: This is a sensitive but crucial topic. Excess weight, especially around the abdomen, puts direct physical pressure on your stomach and that precious LES valve. Losing even a modest amount of weight can reduce reflux symptoms significantly. It’s not about a crash diet, but about consistent, gentle movement and mindful eating to support your whole system.
4. Mind Your Vices: Smoking is disastrous for the LES—it directly weakens the muscle. Alcohol not only relaxes the valve but also stimulates acid production. Cutting back or quitting is one of the most powerful actions you can take.
When to Move Beyond Google and See a Doctor
While lifestyle changes are powerful, they are not always enough. This is where expertise, experience, and authority (the EEAT guidelines in action) come in. You should absolutely consult a doctor if:
-
Your symptoms persist despite over-the-counter medications and lifestyle changes for more than a few weeks.
-
You have difficulty or pain when swallowing (dysphagia), or feel like food gets “stuck.”
-
You experience unexplained weight loss.
-
You have persistent nausea or vomiting.
-
You have chest pain that is severe, especially if it radiates to your arm, neck, or jaw—always rule out heart issues first.
-
You rely on antacids daily.
A doctor, usually a gastroenterologist, might suggest an endoscopy. This sounds scary, but it’s a crucial diagnostic tool. A thin, flexible tube with a camera lets the doctor visually inspect the lining of your esophagus, stomach, and the first part of your small intestine. It’s the only way to accurately diagnose conditions like esophagitis, Barrett’s, or hiatal hernias. In my own journey, getting an endoscopy was the best decision I made; it provided a clear picture and peace of mind.
Treatments can then be tailored. They may include stronger prescription medications like PPIs (Proton Pump Inhibitors) to reduce acid production, or even surgical procedures for a severely weakened LES. The key is having a professional guide you based on evidence, not just internet anecdotes.
Conclusion: From “Isofegas” to Empowered Understanding
That search for “isofegas” is more than just looking up a spelling. It’s the start of a journey toward understanding a hardworking, silent part of your body that deserves attention. Your esophagus is not just a passive pipe; it’s a dynamic organ central to your well-being. By listening to its signals—that burn, that ache, that tightness—you can take proactive steps.
Start with the simple, daily habits: eat mindfully, use gravity wisely, and be kind to your body. If the signals persist, partner with a healthcare professional to get the right diagnosis. Managing esophageal health is often a long-term commitment, but it’s one that pays off in better sleep, more enjoyable meals, and freedom from that nagging, burning worry. You’ve already taken the first step by seeking knowledge. Now you can move forward with clarity and confidence.
Frequently Asked Questions (FAQ)
Q1: What does “isofegas” mean?
“Isofegas” is a common misspelling in online searches for the esophagus, the medical term for the muscular “food pipe” that carries food and liquid from your throat to your stomach.
Q2: What is the main cause of esophageal pain?
The most common cause is acid reflux, where stomach acid flows back up into the esophagus due to a weak or relaxed Lower Esophageal Sphincter (LES). This causes the burning sensation known as heartburn.
Q3: How can I quickly relieve heartburn at home?
Sipping room-temperature water can help dilute acid. Over-the-counter antacids can provide fast, temporary relief. For a natural approach, try chewing sugar-free gum to stimulate saliva, which neutralizes acid. Avoid lying down immediately.
Q4: Can esophageal issues be serious?
Yes, while often manageable, chronic acid reflux (GERD) can lead to serious complications like esophagitis, Barrett’s esophagus, and an increased risk of esophageal cancer. This is why persistent symptoms should be evaluated by a doctor.
Q5: Are there foods that are good for the esophagus?
Yes. Foods that are generally soothing include oatmeal, bananas, melons, ginger, lean poultry, and green vegetables. The goal is to eat non-acidic, low-fat, and high-fiber foods.
Q6: Is difficulty swallowing always a sign of something serious?
Not always, but it should never be ignored. It can be caused by inflammation (esophagitis) or a stricture (narrowing), but it requires a medical evaluation to determine the exact cause and rule out serious conditions.